A PRACTICAL GUIDE TO PERSISTENT PAIN THERAPY
KNOW PAIN PROVIDES ENGAGING, EVIDENCE-BASED LEARNING EXPERIENCES FOR ALL HEALTHCARE PROFESSIONALS. THESE RANGE FROM TAILORED IN-SERVICE TRAINING SESSIONS TO ADVERTISED COURSES.
EMPOWERING FUNCTION THROUGH EDUCATION
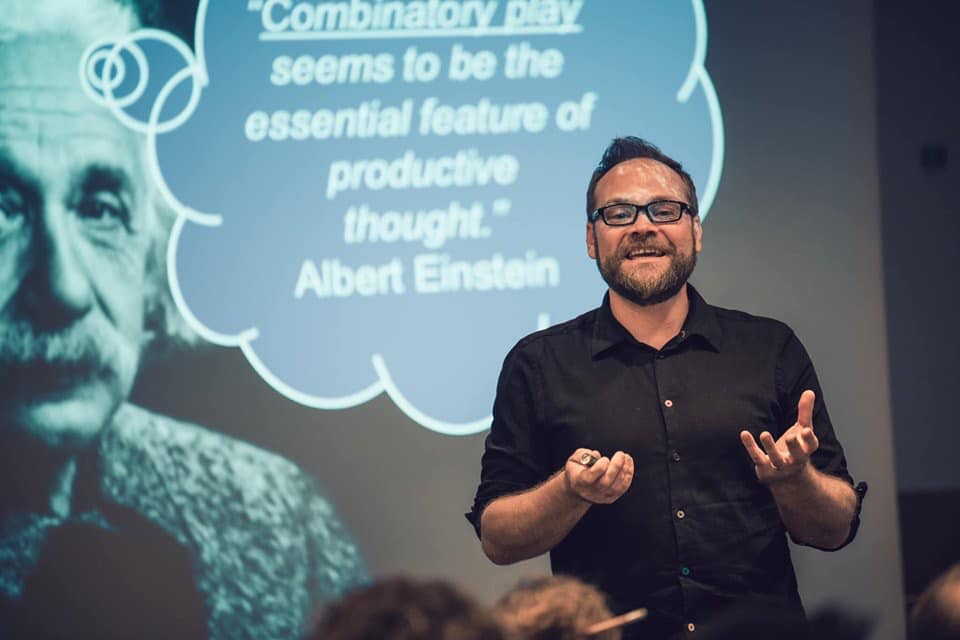
MIKE STEWART
MCSP SRP BSc (Hons) MSc PG Cert (Clin Ed).
“The challenge of successfully managing persistent pain can be one of the most daunting for both clinicians and people living with pain.”
I am a physiotherapist, researcher and university lecturer with over 25 years experience of helping people to overcome pain. I am passionate about providing evidence-based education to a wide variety of health professionals, across a variety of clinical settings, including elite sports, and have advised the International Olympic Committee with regard to pain management
I have an MSc in Education and Physiotherapy, and my published work has received international praise from the leading names in neuroscience.
Know Pain courses have been taught in many countries, and have provided clinicians around the world with practical pain education skills. I hope to meet you soon.
HAPPY CUSTOMERS
Testimonials

Matthew Boyd – Musculoskeletal Physiotherapist. Ottawa, Ontario
“I connect with my patients so much better after taking this course. I get them involved in planning their own rehabilitation and I can see how much more engaged they are. Mike helps you understand how we learn through experience and gives you the practical tools to help your patients learn in the same way. I have used the techniques I learnt with every patient this week. This course is for everyone! Thanks Mike”

Anna Warren – Lead Physiotherapist, England & Wales Cricket Board.
“Mike’s Course was an excellent opportunity for us to explore this complex area as a multidisciplinary team. In the elite sport environment, psychosocial factors are often amplified and education in this area is essential. Both medical staff and coaches got a lot from Know Pain, and I would recommend this to any individuals or teams managing athletes.”
Hannah Watts – Physiotherapist & Pilates Instructor. Whitstable, UK.
“Mike’s course has really made me look and think about the language I use with my patients when talking to them about their pain and the importance of listening. It has enabled me to develop my teaching skills in the explanation of pain so that now I have a better understanding of how to communicate effectively with my patients. The course gives you tools to use with your patients straight away and they work. A fantastic course that I would highly recommend.”